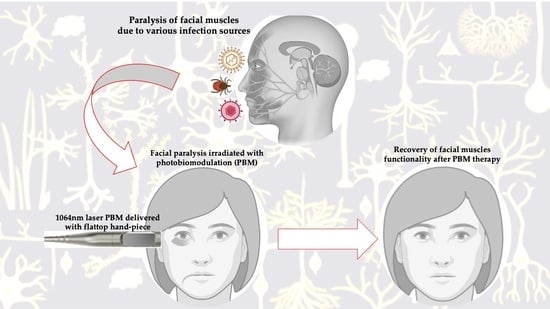
Efficacy of 1064 nm Photobiomodulation Dosimetry Delivered with a Collimated Flat-Top Handpiece in the Management of Peripheral Facial Paralysis in Patients Unresponsive to Standard Treatment Care: A Case Series
Abstract
:1. Introduction
1.1. Role of Oxidative Stress in Pathogenesis of Peripheral Facial Paralysis (PFP)
1.2. Various Diseases Related to PFP and Current Standard Treatment Care
1.2.1. Bell’s Palsy
1.2.2. Lyme Disease
1.2.3. Ramsay Hunt Syndrome
1.3. Photobiomodulation Contributions an Immunomodulator in PFP
1.4. Properties of Collimated Flat-Top Beam Profile
1.5. Rationale in Conducting the Present Case Series Study
2. Materials and Methods
Study Design
3. Case Presentations
3.1. Case 1: Facial Paralysis Related to Bell’s Palsy
3.1.1. Initial Clinical Presentation
3.1.2. Initial Management Prior to PBM Therapy
3.1.3. PBM Treatment Protocol
3.1.4. Results of PBM Therapy
3.2. Case 2: Facial Palsy Related to Lyme Disease
3.2.1. Initial Clinical Presentation
3.2.2. Initial Management Prior to PBM
3.2.3. PBM Treatment Protocol
3.2.4. Results after PBM Therapy and Physiotherapy
3.3. Case 3: Ramsay Hunt Syndrome
3.3.1. Clinical Presentation and Initial Management
3.3.2. Clinical Presentation Prior to PBM Therapy
3.3.3. PBM Dosimetry and Treatment Protocols
3.3.4. Results after PBM Therapy
- During the first week, the patient required less analgesic during the day and was able to progressively sleep more each night. Only slight movement improvement was observed in the eye, mouth and forehead.
- At week 2, more mouth and forehead movements were observed, but little additional eye movement. Longer sleep periods were observed, and pain was intermittent.
- At week 3, good improvement in the movement of the forehead muscles was observed, but there was only marginal improvement in the eye and mouth movements.
- At week 4, the patient was able to have 8 h of uninterrupted sleep due to only a slight neuralgic pain. Additionally, there was more eyebrow movement and tingling at the corner of the mouth and the chin, with some improvement in function.
- At week 6, there was no more neurological pain, which resulted in restful sleep. Lip function had improved, and the patient was able to whistle and eat comfortably. The forehead movement was good, and the patient was able to close his eye voluntarily.
- At week 8, the patient’s face was much more symmetrical, with the eye slowest to improve. The blink reflex was better, and the forehead muscles were moving very well, but there was still numbness and poor tone in the upper lip.
- At week 12, the patient’s smile was almost symmetrical. The blink motion was much faster, and he was feeling mentally and physically stronger. He continued to have restful sleep with no neuralgia.
- At week 20, the subject’s eye and mouth had almost complete movement; his face was symmetrical, and no further treatment was required.
| PBM Treatment Week Number | Functionality Level | Facial Symmetry | Facial Muscles’ Functionality | Total | ||
|---|---|---|---|---|---|---|
| Forehead | Eye | Mouth | ||||
| 0 | Severe | Asymmetric | 6 | 6 | 5 | 17 |
| 1 | Severe | Asymmetric | 5 | 5 | 5 | 15 |
| 2 | Moderately severe | Asymmetric | 4 | 5 | 4 | 13 |
| 3 | Moderate | Asymmetric | 3 | 4 | 4 | 11 |
| 4 | Moderate | Asymmetric | 3 | 4 | 3 | 10 |
| 5 | Moderate | Asymmetric | 3 | 3 | 3 | 9 |
| 6 | Moderate | Asymmetric | 2 | 3 | 3 | 8 |
| 8 | Mild | Mildly asymmetric | 2 | 3 | 2 | 7 |
| 12 | Mild | Symmetric | 1 | 3 | 2 | 6 |
| 20 | Almost normal | Symmetric | 1 | 2 | 2 | 5 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bernal Rodriguez, C.G.; Berlingieri Polho, I.; Azevedo, L.H.; de Paula Eduardo, C. Photobiomodulation Therapy to Treat Facial Paralysis of 8 Years: Case Report. Photobiomodul. Photomed. Laser Surg. 2020, 38, 477–480. [Google Scholar] [CrossRef] [PubMed]
- Coburn, J.; Garcia, B.; Hu, L.T.; Jewett, M.W.; Kraiczy, P.; Norris, S.J.; Skare, J. Lyme Disease Pathogenesis. Curr. Issues Mol. Biol. 2021, 42, 473–518. [Google Scholar] [CrossRef]
- Persson, A.K.; Kim, I.; Zhao, P.; Estacion, M.; Black, J.A.; Waxman, S.G. Sodium channels contribute to degeneration of dorsal root ganglion neurites induced by mitochondrial dysfunction in an in vitro model of axonal injury. J. Neurosci. 2013, 33, 19250–19261. [Google Scholar] [CrossRef] [PubMed]
- Salinas, R.A.; Alvarez, G.; Daly, F.; Ferreira, J. Corticosteroids for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst. Rev. 2010, 3, CD001942. [Google Scholar]
- Minnerop, M.; Herbst, M.; Fimmers, R.; Matz, B.; Klockgether, T.; Wullner, U. Bell’s palsy: Combined treatment of famciclovir and prednisone is superior to prednisone alone. J. Neurol. 2008, 255, 1726–1730. [Google Scholar] [CrossRef] [PubMed]
- Baugh, R.F.; Basura, G.J.; Ishii, L.E.; Schwartz, S.R.; Drumheller, C.M.; Burkholder, R.; Deckard, N.A.; Dawson, C.; Driscoll, C.; Gurgel, R.K.; et al. Clinical practice guideline Bell’s palsy. Otolaryngol. Head Neck Surg. 2013, 149, S1–S27. [Google Scholar]
- Robinson, M.; Hadlock, T.A. Comprehensive facial rehabilitation improves function in people with facial paralysis: A 5-year experience at the Massachusetts Eye and Ear Infirmary. Phys. Ther. 2010, 90, 391–397. [Google Scholar]
- Hadlock, T.A.; Greenfield, L.J.; Wernick-Robinson, M.; Cheney, M.L. Multimodality approach to management of the paralyzed face. Laryngoscope 2006, 116, 1385–1389. [Google Scholar] [CrossRef]
- Tanganeli, J.P.C.; de Oliveira, S.S.I.; da Silva, T.; Fernandes, K.P.S.; Motta, L.J.; Bussadori, S.K. Complete and Fast Recovery from Idiopathic Facial Paralysis Using Laser-Photobiomodulation. Case Rep. Dent. 2020, 2020, 9867693. [Google Scholar] [CrossRef]
- Javaherian, M.; Attarbashi Moghaddam, B.; Bashardoust Tajali, S.; Dabbaghipour, N. Efficacy of low-level laser therapy on management of Bell’s palsy: A systematic review. Lasers Med. Sci. 2020, 35, 1245–1252. [Google Scholar] [CrossRef]
- Poloni, M.M.; Marques, N.P.; Ribeiro Junior, N.V.; Sperandio, F.F.; Hanemann, J.A.C.; de Carli, M.L. Bell’s palsy treated with photobiomodulation in an adolescent: Rare case report and review of the published literature. Int. J. Paediatr. Dent. 2018, 28, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Zhang, X.; Tang, Y.D.; Zhu, J.; Wang, X.H.; Li, S.T. Bell’s Palsy: Clinical Analysis of 372 Cases and Review of Related Literature. Eur. Neurol. 2017, 77, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Chalada, M.J.; Stenos, J.; Bradbury, R.S. Is there a Lyme-like disease in Australia? Summary of the findings to date. One Health 2016, 7, 42–54. [Google Scholar] [CrossRef]
- Radolf, J.D.; Strle, K.; Lemieux, J.E.; Strle, F. Lyme Disease in Humans. Curr. Issues Mol. Biol. 2021, 42, 333–384. [Google Scholar]
- Pacheco, A.; Rutler, O.; Valenzuela, I.; Feldman, D.; Eskin, B.; Allegra, J.R. Positive Tests for Lyme Disease and Emergency Department Visits for Bell’s Palsy Patients. J. Emerg. Med. 2020, 59, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.; Lee, H. Ramsay Hunt syndrome. J. Dent. Anesth. Pain. Med. 2018, 18, 33–337. [Google Scholar] [CrossRef] [PubMed]
- Monsanto, R.D.; Bittencourt, A.G.; Bobato Neto, N.J.; Beilke, S.C.; Lorenzetti, F.T.; Salomone, R. Treatment and prognosis of facial palsy on Ramsay Hunt syndrome: Results based on a review of the literature. Int. Arch. Otorhinolaryngol 2016, 20, 394–400. [Google Scholar] [CrossRef]
- Hashemilar, M.; Ghabili, K.; Shoja, M.M.; Savadi-Oskouei, D.; Keyvani, H. Varicella-zoster virus reactivation from multiple ganglia: A case report. J. Med. Case Rep. 2009, 14, 9134. [Google Scholar] [CrossRef]
- Sweeney, C.J.; Gilden, D.H. Ramsay Hunt syndrome. JNNP 2001, 71, 149–154. [Google Scholar] [CrossRef]
- Poyton, R.O.; Ball, K.A. Therapeutic photobiomodulation: Nitric oxide and a novel function of mitochondrial cytochrome c oxidase. Discov. Med. 2011, 11, 154–159. [Google Scholar]
- Hanna, R.; Dalvi, S.; Benedicenti, S.; Amaroli, A.; Sălăgean, T.; Pop, I.D.; Todea, D.; Bordea, I.R. Photobiomodulation Therapy in Oral Mucositis and Potentially Malignant Oral Lesions: A Therapy Towards the Future. Cancers 2020, 12, 1949. [Google Scholar] [CrossRef] [PubMed]
- El Mobadder, M.; Farhat, F.; El Mobadder, W.; Nammour, S. Photobiomodulation Therapy in the Treatment of Oral Mucositis, Dysphagia, Oral Dryness, Taste Alteration, and Burning Mouth Sensation Due to Cancer Therapy: A Case Series. Int. J. Environ. Res. Public. Health 2019, 16, 4505. [Google Scholar] [CrossRef] [PubMed]
- Karu, T.I. Multiple roles of cytochrome c oxidase in mammalian cells under action of red and IR-A radiation. IUBMB Life 2010, 62, 607–610. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.C.H.; Arany, P.R.; Huang, Y.-Y.; Tomkinson, E.M.; Sharma, S.K.; Kharkwal, G.B.; Saleem, T.; Mooney, D.; Yull, F.E.; Blackwell, T.S.; et al. Low-level laser therapy activates NF-kB via generation of reactive oxygen species in mouse embryonic fibroblasts. PLoS ONE 2011, 6, e22453. [Google Scholar] [CrossRef]
- Hanna, R.; Dalvi, S.; Bensadoun, R.J.; Raber-Durlacher, J.E.; Benedicenti, S. Role of Photobiomodulation Therapy in Neurological Primary Burning Mouth Syndrome. A Systematic Review and Meta-Analysis of Human Randomised Controlled Clinical Trials. Pharmaceutics 2021, 13, 1838. [Google Scholar] [CrossRef]
- Hanna, R.; Bensadoun, R.J.; Beken, S.V.; Burton, P.; Carroll, J.; Benedicenti, S. Outpatient Oral Neuropathic Pain Management with Photobiomodulation Therapy: A Prospective Analgesic Pharmacotherapy-Paralleled Feasibility Trial. Antioxidants 2022, 11, 533. [Google Scholar] [CrossRef]
- Hanna, R.; Dalvi, S.; Bensadoun, R.J.; Benedicenti, S. Role of Photobiomodulation Therapy in Modulating Oxidative Stress in Temporomandibular Disorders. A Systematic Review and Meta-Analysis of Human Randomised Controlled trials. Antioxidants 2021, 10, 1028. [Google Scholar] [CrossRef]
- Zupin, L.; Ottaviani, G.; Rupel, K.; Biasotto, M.; Zacchigna, S.; Crovella, S.; Celsi, F. Analgesic effects of Photobiomodultion Therapy. An in vitro and in vivo study. J. Biophotonics. 2019, 12, e201900043. [Google Scholar] [CrossRef]
- Panhoca, V.H.; Ferreira, L.T.; de Souza, V.B.; Ferreira, S.A.; Simão, G.; de Aquino Junior, A.E.; Bagnato, V.S.; Hanna, R.J. Can photobiomodulation restore anosmia and ageusia induced by COVID-19? A pilot clinical study. Biophotonics 2023, 16, e202300003. [Google Scholar] [CrossRef]
- Hepburn, J.; Williams-Lockhart, S.; Bensadoun, R.J.; Hanna, R. A Novel Approach of Combining Methylene Blue Photodynamic Inactivation, Photobiomodulation and Oral Ingested Methylene Blue in COVID-19 Management: A Pilot Clinical Study with 12-Month Follow-Up. Antioxidants 2022, 11, 2211. [Google Scholar] [CrossRef]
- Hanna, R.; Dalvi, S.; Sălăgean, T.; Pop, I.D.; Bordea, I.R.; Benedicenti, S. Understanding COVID-19 Pandemic: Molecular Mechanisms and Potential Therapeutic Strategies. An Evidence-Based Review. J. Inflamm. Res. 2021, 14, 13–56. [Google Scholar] [CrossRef] [PubMed]
- Hanna, R.; Dalvi, S.; Sălăgean, T.; Bordea, I.R.; Benedicenti, S. Phototherapy as a rational antioxidant treatment modality in COVID-19 management; new concept and strategic approach: Critical review. Antioxidants 2021, 9, 875. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017, 4, 337–361. [Google Scholar] [CrossRef] [PubMed]
- Mosca, R.C.; Ong, A.A.; Albasha, O.; Bass, K.; Arany, P. Photobiomodulation Therapy for Wound Care: A Potent, Noninvasive, Photoceutical Approach. Adv. Skin. Wound Care 2019, 32, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Hanna, R.; Agas, D.; Benedicenti, S.; Laus, F.; Cuteri, V.; Sabbieti, M.G.; Amaroli, A. A comparative study between the effectiveness of 980 nm photobiomodulation, delivered by Gaussian versus flattop profiles on osteoblasts maturation. Front. Endocrinol. Bone Res. 2019, 10, 92. [Google Scholar] [CrossRef] [PubMed]
- Hanna, R.; Dalvi, S.; Amaroli, A.; De Angelis, N.; Benedicenti, S. Effects of photobiomodulation on bone defects grafted with bone substitutes: A systematic review of in vivo animal studies. J. Biophotonics 2020, 14, e202000267. [Google Scholar] [CrossRef]
- Benedicenti, A.; Benedicenti, S. Atlas of Laser Therapy: State of the Art, 4th ed.; Teamwork Media Srl: Villa Carcina, Italy, 2016; pp. 141–152. [Google Scholar]
- Khan, I.; Arany, P.R. Dosimetry for photobiomodulation therapy: Response to Sommers et al. Ann. Transl. Med. 2016, 4, 208. [Google Scholar] [CrossRef]
- Amaroli, A.; Ferrando, S.; Hanna, R.; Gallus, L.; Benedicenti, A.; Scarfì, S.; Pozzolini, M.; Benedicenti, S. The photobiomodulation effect of higher-fluence 808-nm laser therapy with a flat-top handpiece on the wound healing of the earthworm Dendrobaena veneta: A brief report. Lasers Med. Sci. 2018, 33, 221–225. [Google Scholar] [CrossRef]
- Hanna, R.; Dalvi, S.; Tomov, G.; Hopper, C.; Rebaudi, F.; Rebaudi, A.L.; Bensadoun, J.R. Emerging potential of phototherapy in management of symptomatic oral lichen planus: A systematic review of randomised controlled clinical trials. JOB 2023, 16, e202300046. [Google Scholar] [CrossRef]
- Skondra, F.G.; Koletsi, D.; Eliades, T.; Farmakis, E.T.R. The Effect of Low-Level Laser Therapy on Bone Healing After Rapid Maxillary Expansion: A Systematic Review. Photomed Laser Surg. 2018, 36, 61–71. [Google Scholar] [CrossRef]
- Kalhori, K.A.M.; Vahdatinia, F.; Jamalpour, M.R.; Vescovi, P.; Fornaini, C.; Merigo, E.; Fekrazad, R. Photobiomodulation in Oral Medicine. Photobiomodul Photomed. Laser Surg. 2019, 37, 837–861. [Google Scholar] [CrossRef]
- Alayat, M.S.M.; Elsodany, A.M.; El Fiky, A.A.R. Efficacy of high and low level laser therapy in the treatment of Bell’s palsy: A randomized double blind placebo-controlled trial. Lasers Med. Sci. 2014, 29, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Ho, A.L.; Scott, A.M.; Klassen, A.F.; Cano, S.J.; Pusic, A.L.; Van Laeken, N. Measuring quality of life and patient satisfaction in facial paralysis patients: A systematic review of patient-reported outcome measures. Plast. Reconstr. Surg. 2012, 130, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Kandakurti, P.K.; Shanmugam, S.; Basha, S.A.; Sampath, K.; Suganthirababu, P.; Gopal, K.; George, G.S. The effectiveness of low-level laser therapy combined with facial expression exercises in patients with moderate-to-severe Bell’s palsy: A study protocol for a randomised controlled trial. Int. J. Surg. Protoc. 2020, 24, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Eviston, T.J.; Croxson, G.R.; Kennedy, P.G.E.; Hadlock, T.; Krishnan, A.V. Bell’s palsy: Aetiology, clinical features and multidisciplinary care. J. Neurol. Neurosurg. Psychiatry 2015, 6, 1356–1361. [Google Scholar] [CrossRef]
- Masoumipoor, M.; Jameie, S.B.; Janzadeh, A.; Nasirinezhad, F.; Kerdari, M.; Solemani, M. Effects of 660nm Low Level Laser Therapy on Neuropathic Pain Releif Following Chronic Costriction Injury in Rat Sciatic Nerve. Arch. Neurosci. 2014, 1, 76–81. [Google Scholar] [CrossRef]
- Panhóca, V.H.; Nogueira, M.S.; Bagnato, V.S. Treatment of facial nerve palsies with laser and endermotherapy: A report of two cases. Laser Phys. Lett. 2020, 18, 015601. [Google Scholar] [CrossRef]
- Laakso, L.; Richardson, C.; Cramond, T. Factors affecting low level laser therapy. Aust. J. Physiother. 1993, 39, 95–99. [Google Scholar] [CrossRef]
- Aub, L.; Schmitz, C. Comparison of the Penetration Depth of 905 nm and 1064 nm Laser Light in Surface Layers of Biological Tissue Ex Vivo. Biomedicines 2023, 11, 1355. [Google Scholar] [CrossRef]
- Har-Shai, Y.; Bodner, S.R.; Egozy-Golan, D.; Lindenbaum, E.S.; Ben-Izhak, O.; Mitz, V.; Hirshowitz, B. Mechanical properties and microstructure of the superficial musculoaponeurotic system. Plast. Reconst. Surg. 1996, 98, 59–70. [Google Scholar] [CrossRef]












| Device Specifications | Manufacturer | Fotona, Ljubljana, Slovenia |
| Model identifier | LightWalker | |
| Emitters Type | Nd:YAG laser | |
| Laser aiming beam | 532 nm | |
| Medical/laser class | IV | |
| Beam delivery system | Fibre | |
| Probe design | Single probe | |
| Beam profile | Collimated flat-top | |
| Beam divergence full angle | 0° | |
| Irradiation parameters | Wavelength | 1064 nm |
| Therapeutic power output | 3200 mW | |
| Emission mode | Pulsed | |
| Pulse width (microseconds) | 100 | |
| Beam spot size at target (cm2) | 6 cm2 | |
| Irradiance at target (mW/cm2) | 533 mW/cm2 | |
| Energy per pulse (J) | 320 mJ | |
| Energy (J) per spot | 192 J | |
| Fluence (J/cm2) per point | 32 J/cm2 | |
| Duration of irradiation (s) | 60 s | |
| Area irradiated (cm2) | 6 cm2 |
| Number of irradiated points | 7 | |
| Laser–tissue distance | In contact | |
| Application technique | Spotting technique | |
| Frequency of treatment sessions time | First month | 12 sessions |
| Time interval between treatment sessions | 1st, 3rd and 5th | |
| Total number of treatments and duration | 27 during 6 months | |
| PBM Treatment Week Number | Functionality Level | Facial Symmetry | Facial Muscles’ Functionality | Total | ||
|---|---|---|---|---|---|---|
| Forehead | Eye | Mouth | ||||
| 0 | Severe | Asymmetric | 5 | 3 | 5 | 13 |
| 1 | Severe | Asymmetric | 5 | 3 | 5 | 13 |
| 2 | Severe | Asymmetric | 5 | 3 | 5 | 13 |
| 3 | Severe | Asymmetric | 5 | 3 | 5 | 13 |
| 5 | Moderate | Asymmetric | 4 | 3 | 5 | 12 |
| 7 | Moderate | Asymmetric | 4 | 3 | 4 | 11 |
| 11 | Moderate | Asymmetric | 3 | 3 | 4 | 10 |
| 15 | Moderate | Asymmetric | 3 | 2 | 3 | 8 |
| Number of irradiated points | 12 | |
| Laser–tissue distance | In contact | |
| Application technique | Spotting technique | |
| Frequency of treatment sessions | First month | 12 sessions |
| Time interval between treatment sessions | 1st,3rd and 5th day | |
| Total number of treatments and duration | 22 during 4 months | |
| PBM Treatment Week Number | Functionality Level | Facial Symmetry | Facial Muscles’ Functionality | Total | ||
|---|---|---|---|---|---|---|
| Forehead | Eye | Mouth | ||||
| 0 | Paralysis | Asymmetric | 6 | 6 | 6 | 18 |
| 1 | Severe | Asymmetric | 6 | 6 | 5 | 17 |
| 2 | Severe | Asymmetric | 5 | 5 | 4 | 14 |
| 3 | Moderate | Asymmetric | 4 | 4 | 3 | 11 |
| 4 | Moderate | Asymmetric | 3 | 4 | 3 | 10 |
| 5 | Moderate | Asymmetric | 3 | 4 | 2 | 9 |
| 8 | Mild | Mildly asymmetric | 2 | 4 | 2 | 8 |
| 9 | Almost normal | Mildly asymmetric | 2 | 3 | 2 | 7 |
| 13 | Almost normal | Symmetric | 2 | 2 | 2 | 6 |
| 23 | Normal | Symmetric | 1 | 1 | 1 | 3 |
| Number of irradiated points | 11 | |
| Laser–tissue distance | In contact | |
| Application technique | Spotting technique | |
| Frequency of treatment sessions time interval and duration | First month | 22 |
| Second month | 11 | |
| Third month | 7 | |
| Fourth month | 4 | |
| Fifth month | 4 | |
| Total number of treatments | 48 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zarkovic Gjurin, S.; Pang, J.; Vrčkovnik, M.; Hanna, R. Efficacy of 1064 nm Photobiomodulation Dosimetry Delivered with a Collimated Flat-Top Handpiece in the Management of Peripheral Facial Paralysis in Patients Unresponsive to Standard Treatment Care: A Case Series. J. Clin. Med. 2023, 12, 6294. https://doi.org/10.3390/jcm12196294
Zarkovic Gjurin S, Pang J, Vrčkovnik M, Hanna R. Efficacy of 1064 nm Photobiomodulation Dosimetry Delivered with a Collimated Flat-Top Handpiece in the Management of Peripheral Facial Paralysis in Patients Unresponsive to Standard Treatment Care: A Case Series. Journal of Clinical Medicine. 2023; 12(19):6294. https://doi.org/10.3390/jcm12196294
Chicago/Turabian StyleZarkovic Gjurin, Sonja, Jason Pang, Mihael Vrčkovnik, and Reem Hanna. 2023. "Efficacy of 1064 nm Photobiomodulation Dosimetry Delivered with a Collimated Flat-Top Handpiece in the Management of Peripheral Facial Paralysis in Patients Unresponsive to Standard Treatment Care: A Case Series" Journal of Clinical Medicine 12, no. 19: 6294. https://doi.org/10.3390/jcm12196294